
Virtual remote appointments are available. Contact us for a video telehealth evaluation.

All appointments conducted by our Board Certified doctor and not assistants or non-physician providers.
A spermatocele is a fluid containing cyst that develops within the epididymis, the coiled tube located on the back of the testicle. While generally non-painful, spermatoceles can cause discomfort and impact fertility. Traditional treatment options include surgical excision, but sclerotherapy offers a less invasive approach.
Spermatocele Formation and Associated Risks:
A spermatocele forms when there is a blockage in the epididymal ducts, leading to the accumulation of fluid and sperm. These cystic masses are typically benign but can grow in size, causing pain or discomfort. While not directly linked to serious health risks, complications such as infection or rupture may occur. Additionally, spermatoceles may impact fertility by causing obstruction to the normal flow of sperm.1
Spermatocele Treatment Options
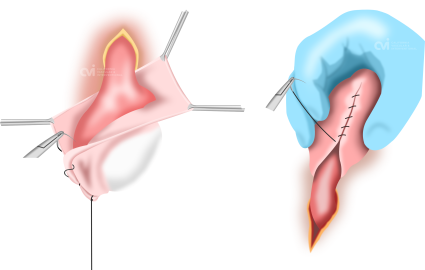
Spermatocele Surgical Excision
The primary conventional treatment for spermatoceles involves surgical removal through excision. While effective in eliminating the cyst, surgery comes with inherent risks such as infection, bleeding, and postoperative pain. Moreover, the recovery period may involve restrictions on physical activities, impacting daily life.2
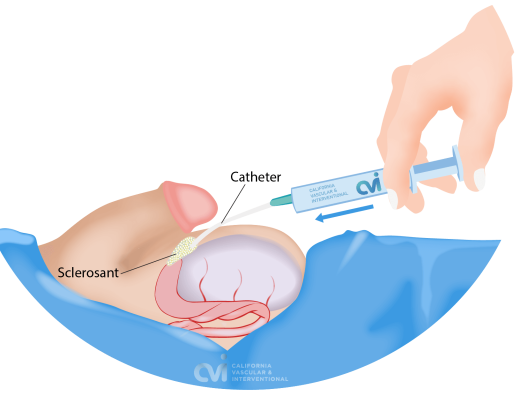
Spermatocele Sclerotherapy
Sclerotherapy is a minimally invasive procedure in treating various cystic conditions, including cysts in the kidney and liver. The procedure involves the injection of a sclerosing agent directly into the cystic mass through a catheter after aspiration of the contents. This causes the cyst to collapse without the need for surgical excision. Sclerotherapy however may require multiple sessions. In larger organs such as the kidney, our specialist leaves a drainage catheter in the cystic cavity that patients go home with. Repeat sclerotherapy treatments are performed through the catheter until the cyst resolves. In the testicle however a catheter is not left in place because of the small organ size. The catheter is removed after each sclerotherapy treatment.
Spermatocele Sclerotherapy Benefits Over Surgery
Sclerotherapy offers several potential advantages over surgery. Firstly, it is a less invasive procedure that requires no incisions, reducing the risks associated with open surgery. The recovery time is one day if any, and the procedure is performed in our office. Additionally, sclerotherapy minimizes the risk of complications such as infection and bleeding, commonly associated with surgical interventions.3
Comparing Risks: Sclerotherapy vs. Surgery:
Postoperative Pain and Recovery Time
One of the primary advantages of spermatocele sclerotherapy is the reduced postoperative pain compared to surgical excision. Surgery often involves incisions and tissue manipulation, leading to more significant discomfort during the recovery period. Sclerotherapy, being less invasive and suture free, results in fast recovery and minimal post-procedural pain.
Complications
Surgical procedures, particularly in the delicate genital area, carry inherent risks of complications such as infection, bleeding, and scrotal hematoma. Sclerotherapy, being a catheter-based intervention, minimizes the risk of infection and bleeding. Complications associated with sclerotherapy are generally rare but can include local discomfort or swelling at the injection site.
Impact on Fertility
The impact of spermatocele treatment on fertility is a crucial consideration. Surgical excision, while effective in removing the cyst, might pose a risk to the delicate structures of the epididymis, potentially affecting sperm flow. Sclerotherapy, by contrast, aims to collapse the cyst without direct manipulation of surrounding tissues, theoretically minimizing the impact on sperm flow and fertility.4
Spermatocele Treatment Satisfaction
Both sclerotherapy and surgery have been shown to effectively alleviate symptoms associated with spermatoceles. However, the less invasive nature of sclerotherapy might contribute to higher patient satisfaction due to a smoother recovery process and reduced post-procedural discomfort.
A critical aspect often overlooked is the impact of the treatment on the patient's overall quality of life. Sclerotherapy, by virtue of being less traumatic and associated with fewer complications, may contribute positively to the patient's psychological well-being during the recovery phase. The ability to resume regular activities sooner and with less discomfort can enhance the overall experience for individuals undergoing spermatocele treatment.5
While both spermatocele sclerotherapy and surgical excision aim to alleviate symptoms and improve the patient's quality of life, the choice between the two should be individualized. Sclerotherapy offers a less invasive alternative with potential advantages in terms of reduced postoperative pain, quicker recovery, and fewer complications.
Our doctor has his own ultrasound guided technique and many years of experience that has allowed many patients to achieve successful outcomes. Contact us today to setup an appointment with our doctor to review your medical records and expected outcomes for your particular spermatocele.
Contact Us Today
Request an appointment to meet with our embolization specialist who will review your imaging and medical records to determine if you are a good candidate and outcomes you can expect. Consultations can be via an online video telehealth platform or in person at one of the offices in Los Angeles, Orange County or San Diego, depending on the doctor’s availability. Why should you choose us? Read here.
References:
- Paick SH, Park HK, Kim HH, Lee SW, Song SU. A clinical study of spermatoceles. Int J Urol. 1999;6(11):553-557.
- Schwarzer JU, Nieden S, Sticht G, et al. Complete excision of large spermatoceles as a therapeutic option. World J Mens Health. 2019;37(2):239-244.
- Flanigan RC, Reda DJ, Wasson JH, Anderson RJ, Abdellatif M, Bruskewitz RC. 5-year outcome of surgical resection and watchful waiting for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol. 1998;160(1):12-16.
- Paick SH, Park HK, Kim HH, Lee SW, Song SU. A clinical study of spermatoceles. Int J Urol. 1999;6(11):553-557.
- Ludemann JP, McAninch JW. Acute testicular disorders. Surg Clin North Am. 1997;77(6):1471-1492.
